Packard Center and Project ALS host workshop to share knowledge on culturing human neurons as an essential research tool
From April 28–30, more than forty leading researchers gathered in Washington, D.C., at the invitation of the Robert Packard Center for ALS Research and Project ALS to discuss the critical challenges of accurately modeling ALS in a dish. The meeting aimed to harness the potential of new technologies to develop better tools for understanding how ALS develops and to accelerate the path toward effective treatments.
ALS is a disease that targets motor neurons—the nerve cells responsible for sending signals from the brain to the muscles, enabling everything from walking to breathing. In ALS, motor neurons progressively die, followed closely by the muscles they control. What causes these motor neurons to perish is the million-dollar question—one that has been difficult to answer, as scientists can’t easily “biopsy” living motor neurons to study them directly.
The Challenge
Almost 20 years ago, scientists discovered how to reprogram adult cells from the skin or blood into a stem cell-like state. These reprogrammed cells, with their genetic clocks reset, can be coaxed into many of the body’s adult cell types, including neurons. In fact, through funding from Project ALS, ALS was one of the first diseases studied using this reprogramming system. Yet many years later, researchers still lack a single, well-defined cell model of ALS that accurately represents how the disease develops in most people living with ALS.
Moreover, only 5-10% of ALS cases link to known genetic mutations. The vast majority are considered sporadic, meaning they arise spontaneously and without an identifiable cause. Although researchers identified up to 40 additional genes that may play a role in the disease, sporadic cases remain the most common and least understood, making them the greatest blind spot in ALS research.
“Mouse models are completely failing us here,” said Jeffrey Rothstein, MD, PhD, the Packard Center’s founder and director, during his passionate introduction to the workshop. “Mice are completely irrelevant for sporadic ALS, which is the most pressing issue for studying the mechanism behind this disease.” Rothstein expressed both his frustration at the lack of progress in the field for sporadic ALS and his hope for what the assembled experts could accomplish together at the event.
The Community
At the launch of the workshop, Project ALS Co-Founder Valerie Estess shared how she and her family founded the organization when her sister, Jenifer, was diagnosed with ALS at 35 years old. Estess conveyed the progress made in creating ALS cell models, citing many of the workshop’s participants in those efforts.
“ALS research faces new challenges, but know that at the Packard Center and Project ALS, we will support you,” said Estess. “Here’s to a great working session.”
 Estess then told the story of EJ McLaren, whom she met as a young boy when his father was diagnosed with ALS. McLaren traveled to New York to visit the Jenifer Estess Lab for Stem Cell Research and see his father’s cells under a microscope. Now, ten years after losing his father, he is pursuing his PhD at Duke University and spoke to the workshop participants about his trajectory from caregiver to researcher.
Estess then told the story of EJ McLaren, whom she met as a young boy when his father was diagnosed with ALS. McLaren traveled to New York to visit the Jenifer Estess Lab for Stem Cell Research and see his father’s cells under a microscope. Now, ten years after losing his father, he is pursuing his PhD at Duke University and spoke to the workshop participants about his trajectory from caregiver to researcher.
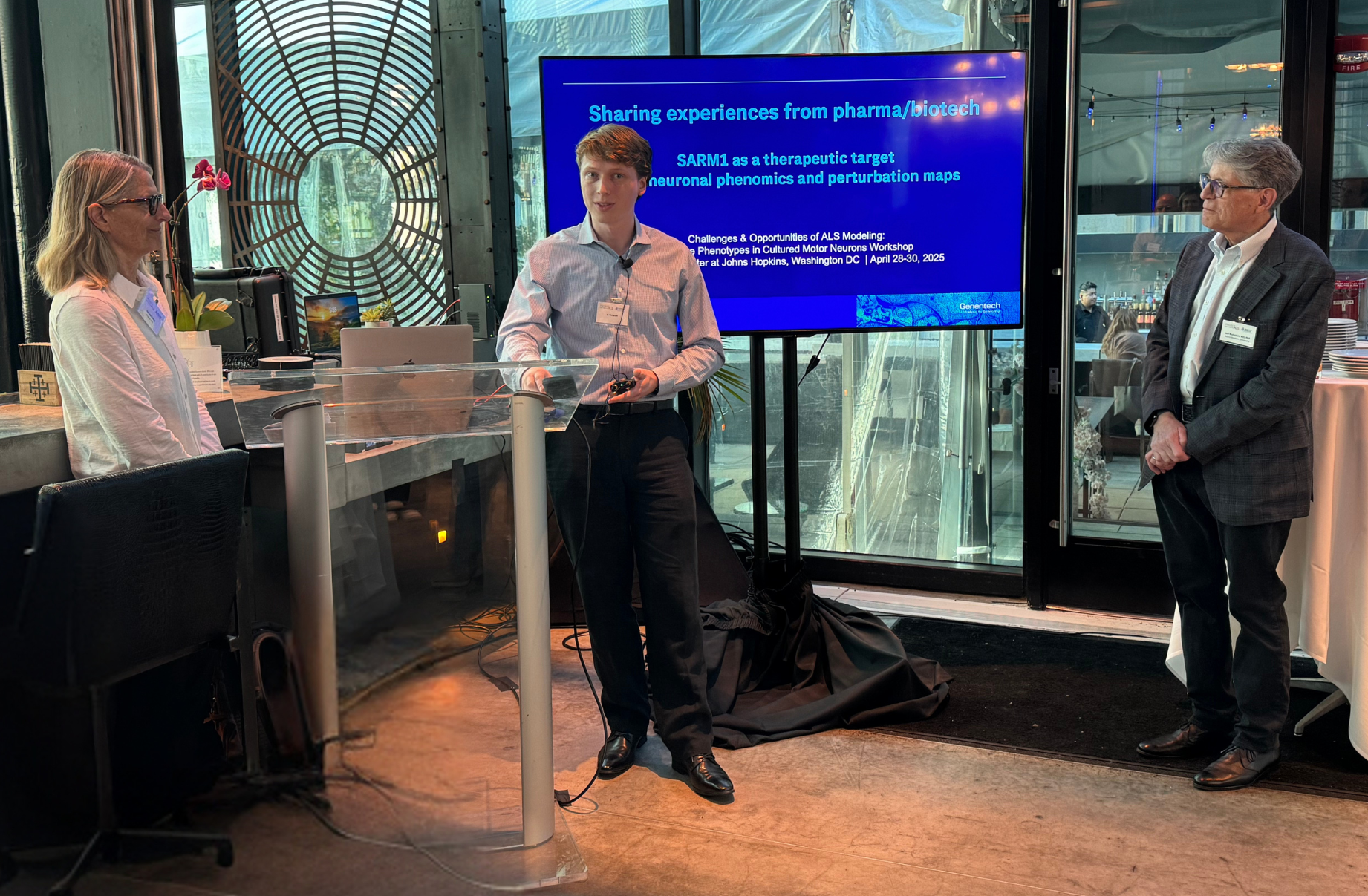
Keynote speaker Casper Hoogenraad, PhD, of Genentech, shared insights into the pursuit of one potential ALS drug target, in part by using patients’ reprogrammed stem cells for their studies. In addition, he shared about ongoing drug development efforts, using AI and machine learning to evaluate how genetic changes and/or drug treatments impact the neurons generated from these reprogrammed stem cells at a large scale (more than 1,500 different experimental conditions at once!).
ALS Cell Models
Many researchers at the workshop presented work using cells containing a handful of well-known ALS genetic mutations, such as SOD1, C9ORF72, and FUS. They reported on the types of cells used—each with advantages, challenges, and ideal applications. These included everything from immature neurons to highly specialized motor neurons derived from different regions of the body.
One researcher used precursor cells derived from reprogrammed stem cells. These cells come from the skin’s connective tissue, known as fibroblasts, and can be used for simple drug screens to identify candidate drugs that reverse ALS-like traits in a dish.
Another researcher reported converting fibroblasts directly into neurons by skipping the reprogramming stem cell stage altogether. Yet another scientist created neurons that mirror those most affected by ALS, such as those controlling the jaw, tongue, and throat, and compared them to neurons that remain largely resistant to the disease, like those that control movement of the eye.
Determining what protects the eye motor neurons from damage, and why some neurons are more vulnerable, could reveal mechanisms that may lead to new therapeutic strategies.
“In the preclinical pipeline, we need better ALS cell models to identify more appropriate therapeutic targets and reduce the risk for drug developers—so they’re not playing a high-stakes game of roulette,” said presenter Steve Finkbeiner, MD, PhD, of the University of California, San Francisco.
Even in cells carrying known ALS mutations, clear disease characteristics don’t always appear on their own. To coax these symptoms, researchers treat the cells with chemicals or drugs that disrupt their normal function. While healthy cells typically mount a predictable response to stressors like these, those from individuals with ALS may respond abnormally, even beginning to show signs of the disease.
One of the most common markers used to assess if a neuron has ALS characteristics is TDP-43. Normally located in the cell’s nucleus where the DNA resides turning on certain genes, this protein marker can move outside of the nucleus in stressed or diseased cells. In more severe cases, TDP-43 forms toxic clumps in the cell, a hallmark of ALS disease. Researchers can also mimic ALS by “feeding” TDP-43 clumps to healthy neurons, which then can spread and make the neurons sick.
Separately, researchers are developing cell lines derived from people living with sporadic ALS. Notably, the Packard Center’s Answer ALS initiative generated a repository of over 1,000 such lines. However, considerable variability exists between different lines, even those derived from the same person.

Challenges
Growing neurons in the lab presents universal challenges. Chief among them, keeping cells alive and preventing changes in shape and structure over time. Several researchers shared strategies for optimizing growth conditions to address these issues.
A major concern among workshop participants was the role biological age may play in cell behavior. Gene and protein levels may vary depending on how “old” the neurons are. As ALS is a disease of aging, the cell’s internal clock needs to advance to mimic disease conditions. Yet the field lacks a standardized method for measuring or controlling the age of neurons grown in culture.
“Conceptually, we’re trying to model a disease that unfolds over decades in an organism, but we’re not letting the cells naturally mature through normal developmental stages,” said Esteban Mazzoni, PhD, of New York University. “It’s a miracle that we can even measure changes in these cells.”
The Wishlist
After thoughtful discussion, the group reached consensus that developing a shared set of resources would be highly valuable for the ALS research community.
One proposal was to create a simple, standardized assay to assess the “age” of neurons, ensuring consistency across laboratories. This could involve measuring specific, predictable markers on DNA or the proteins that package it within the nucleus.
 Another idea was to identify a set of markers that define an ALS cell’s unique signature. Using tools like machine learning or AI, researchers could develop a cellular fingerprint of ALS, potentially allowing for detection decades before symptoms appear. This could be especially impactful for children of people living with ALS, who might benefit from early screening and risk factor-reducing interventions.
Another idea was to identify a set of markers that define an ALS cell’s unique signature. Using tools like machine learning or AI, researchers could develop a cellular fingerprint of ALS, potentially allowing for detection decades before symptoms appear. This could be especially impactful for children of people living with ALS, who might benefit from early screening and risk factor-reducing interventions.
A final suggestion was to establish a small set of well-characterized cell lines—including both genetic and sporadic ALS cases—that would be easily accessible to researchers worldwide. Streamlining administrative hurdles would ensure easy access to these cell lines generated under consistent conditions with known data, saving time and providing more standardization in the field.
Overall, the dynamic, free-flowing discussion was unparalleled. And the momentum didn’t end when the meeting ended. Working groups are already forming to move these ideas forward, with the goal of translating them into reality.
“Workshops like these are critical to our mission to empower collaborative and innovative research that advances our fundamental understanding of ALS by engaging and supporting the global research community,” said Packard Center’s Scientific Director Christine Vande Velde, PhD. “Working with our partners, we share a collective vision — to significantly alter the course of ALS.”
Written by Vanessa McMains, PhD